Blogs are written by COST Actions
Sexual medicine is an immense field that deals with disorders of sexual health of individuals throughout the course of life. Due to its broad scope, a comprehensive approach to the subject is largely non-existent: research is in short supply and few medical educators are qualified to teach the subject. COST Action ESMN aims to exchange research results produced by different disciplines in order to find commonalities in concepts and approaches to sexual medicine. This will serve as the foundation for identifying shared concepts and definitions, and the start of joint interdisciplinary research. It will also form the conceptual groundwork for developing curricula for further university education at a European standard of qualification and recognition.
The background
One of the main deliverables of the ESMN COST Action is to develop a model curriculum in Sexual Medicine for undergraduate university medical and psychological education in Europe. The curriculum will be supported by dedicated educational material developed be members of ESMN.
Sexual Health and Sexual Medicine are not part of most curricula in medical schools and psychology teaching institutions, although future physicians and psychotherapists and counsellors are confronted with people having sexual problems and suffering from sexual dysfunctions or disorders. This demand for care goes across all disciplines because sexuality is an essential part of health and quality of life
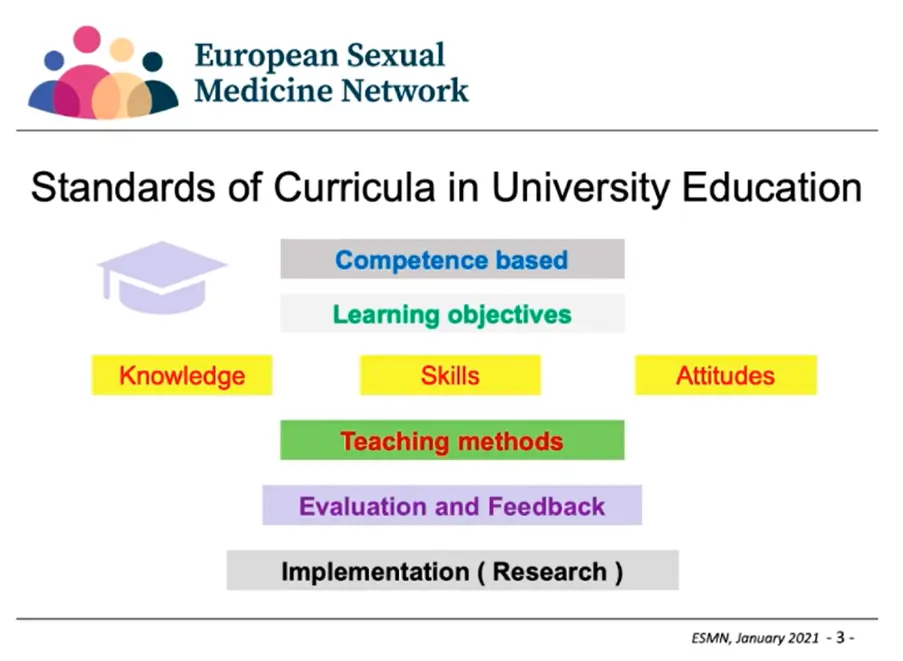
The ESMN curriculum should provide basic education and training as integrated part of the general curriculum thus providing the knowledge, skills and attitudes to respond to sexual health issues from prevention, counselling to specialist referral. It is about basic care and not meant as a subspecialty among other specialties. Existing curricula are often focusing on special interests of the respective specialists.
How did we do it?
We first defined the basic competence students should gain to address sexual issues with their patients or clients. What is the knowledge they need and the skills they have to respond to the sexual health needs and problems of their future patients or clients. We defined eight topics students should gain knowledge about and the communication and counselling skills specific for sexual health care
One of the big challenges was that we could for a longer period not meet face to face to discuss and elaborate the material. The virtual exchange in producing slides, texts, references etc was difficult especially taking account the input from different specialists with their specific views which had to be integrated into a didactic coherent material.
Creating the best possible curriculum for Sexual Medicine
In designing curriculum members decided it was important to structure the course to cover three key areas: knowledge, skills, and attitudes.
1. Knowledge
Following a thorough analysis we concluded that the knowledge part of the curriculum should consider 8 key topics:
This knowledge is best transmitted to students through a series of lectures, manuscripts (slides and text), and videos. The Action is currently preparing these materials that will be available to those who are interested in using them in their own teaching efforts at different faculties all over Europe.
2. Skills
The skills training part of the curriculum focuses on the specific challenges regarding communication and counselling on sexual and reproductive health. It is important to address sexual health issues in a patient centered way and when addressing issue in a couple it is important to respectfully consider both partners perspectives.
Patient centered communication in Sexual Medicine can include a whole range of topics such as reassuring patients of privacy and explaining confidentially, making efforts to ensure trust and openness, and avoiding assumptions (on topics like sexual orientation, gender identity, monogamy, sexual activities, or age-related practices).
Video 1 Sexual history taking based on the concept of the variety of sexual expression
Video 2 How to help patients presenting a sexual problem in the consultation
3. Attitudes
In the final part of the course it is key that undergraduate students are also made aware of their beliefs and values regarding sexuality and the impact of these on their care for patients. It will also be important for students to understand the large variability of sexual expressions and develop an open non-judgmental attitude.
Learning objectives of the curriculum
Having participated in the course undergraduate student should be able to successfully:
- Perform a sexual history including assessment of sexual health risks and sexual concerns, encourage questions and create an open confidential non-judgemental atmosphere following the principles of patient centred communication and patient/professional relationship based on trust and respect
- Counsel patients on sexual health protection and promotion (contraception, STIs, violence)
- Encourage questions and inform and educate patients and their partners about the basic facts of the anatomy, physiology and psychology of the human sexual response in women and men and their partners
- Address proactively sexual wellbeing and sexual function in a respectful non-invasive manner
- Take care of patients with sexual problems and concerns in general as well as in the context of disease
- By practising patient or couple centred counselling based on proactive respectful asking, empathic listening and providing evidence based information with respect to the problem presented
- By informing patients (couples) about therapeutic options and provide referral if desired by the patient (couple)
- Communicate, educate and counsel non only the individual patient but have the skills to include the partner in the process (dyadic setting)
The next steps
We are currently in the process of finalising the knowledge and skills part of the curriculum and preparing the part on attitudes. The materials will then be presented to the European Professional Organisations responsible for education and accreditation in Sexual Medicine to establish collaboration regarding continuous evaluation, improvement, and implementation in university programs and curricula with the help of the European Parliament.
